Are You Looking For a Physiotherapist In Christchurch?
Why Book at Muscle People Physiotherapy?
Expert Care. Proven Results. Convenient Location.
When it comes to your health, you deserve the best and that’s exactly what we deliver.
At Muscle People Physiotherapy, we combine clinical expertise with genuine care to provide results-driven physiotherapy that puts you first.
Our experienced team doesn’t just treat symptoms, we pride ourselves on our pain to performance approach to client care where we take the time to understand the root cause of your pain and create a personalised plan to help you move better, feel stronger and get back to what you love. Our model is relieving symptoms, restoring function and improving your long term health.
Because it's not just about living longer—it's about living well. Prioritising your health span means staying active and independent for as many years as possible.
Make your health a priority and book an appointment with one of our expert physios and take the first step towards better health.

Muscle People Physiotherapy was established by Laurie Moore in 1998 and has consistently provided a high standard of Physiotherapy care to Christchurch residents and professionals, as well as the broader community.

What Sets Us Apart?
We have been serving Christchurch for over 25 years, we know our community and its needs.
Our experienced physiotherapists are highly trained in low back and neck pain, knee and shoulder pain to to sports injuries and post-surgical rehab. We also offer acupuncture, pelvic health, vestibular physiotherapy, hypermobility management, and headache and migraine treatment. Our niche expertise means you won’t need multiple referrals.
We pride ourselves on our pain to performance approach to client care; relieving your pain, rebuilding your strength and exceeding your goals.
We use high-end assessment tools and innovative equipment such as Real Time ultrasound, VALD DynaMos, ForceDecks, Force Frame and HumanTrak Force Plates, Shockwave Therapy, Rip60s, Oovs, SurfSets and full commercial gym facilities to accurately diagnose, track progress and personalise treatment.
How Can We Help?
At Muscle People Physiotherapy we treat a wide range of conditions from everyday aches to complex injuries. Whether you're dealing with a recent injury or something that’s been nagging you for a while, our experienced physiotherapists can help you understand the cause and work towards lasting relief.
We commonly help clients with:
Back pain – from stiffness and postural strain to disc injuries and sciatica
Neck pain & headaches – including tension, whiplash and desk-related strain
Shoulder pain – such as rotator cuff issues, bursitis and frozen shoulder
Knee pain – from ligament injuries and arthritis to patellofemoral pain
Hip & pelvic pain – affecting movement, stability or sleep
Ankle & foot problems – including sprains, Achilles issues and plantar fasciitis
Post-surgical recovery – regain strength and mobility after orthopaedic surgery
Sports injuries – from sprains and strains to overuse injuries
Balance and dizziness issues – including BPPV and vestibular dysfunction

Confused about your pain and not sure what to do?
Get clear, professional advice in our free downloadable information packs
Back Pain
Understand why back pain happens and how to help it
Shoulder Pain
Understand why shoulder pain happens and how to help it
Knee Pain
Understand why knee pain happens and how to help it
Latest Tips and Advice

Why Physiotherapy Is So Effective for Back Pain – Insights from Muscle People Physiotherapy Christchurch
New Blog Post Description ...more
Physiotherapy
August 02, 2025•2 min read
Contact us today to speak with our friendly team and find out how we can help you feel your best

Muscle People Physiotherapy is powered by Vitala Health, a group of Allied Health Practices across New Zealand and Australia.
Vitala Health provides clinical solutions that supports clients health and lifestyle needs through best practice treatment, premium facilities, education and ongoing commitment to customer service. Learn more about Vitala Health
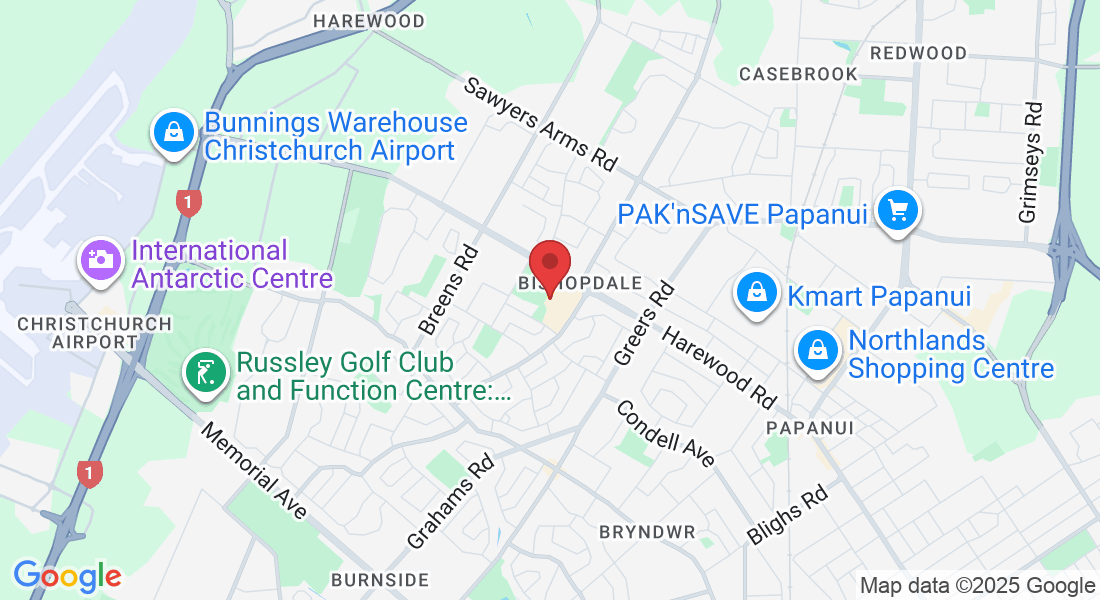
Bishopdale
03 360 3606
13A Bishopdale Ct, Bishopdale, Christchurch 8053
Monday 8:00am-8:00pm
Tuesday 9:00am-6:00pm
Wednesday 8:00am-8:00pm
Thursday 8:00am-8:00pm
Friday 8:00am-7:20pm
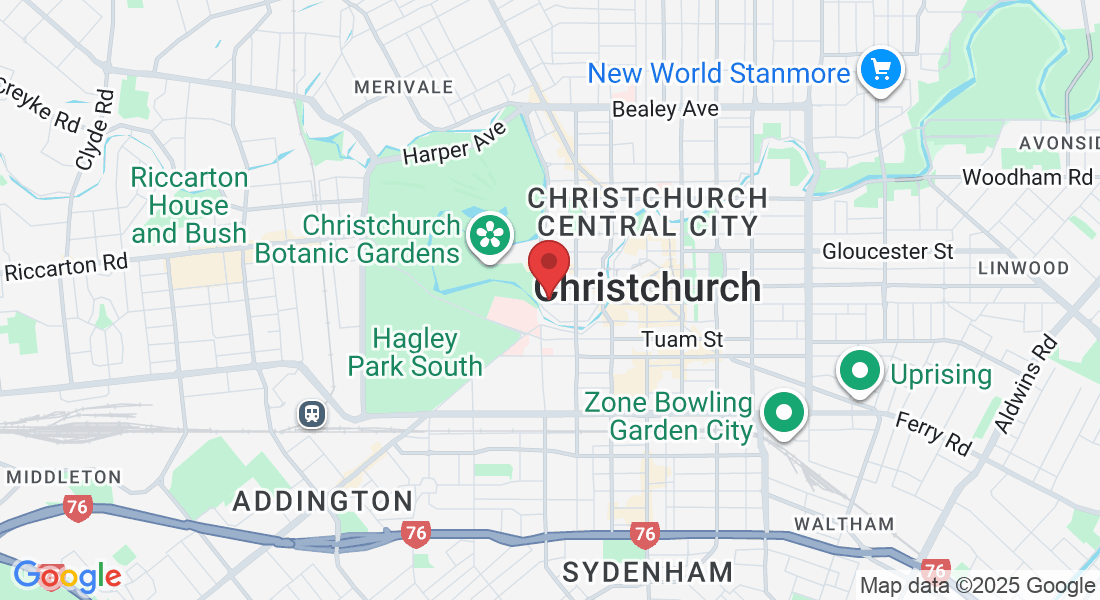
City
03 961 0236
1 Cashel St,
Christchurch, 8013
Monday 8:00am-6:30pm
Tuesday 9:00am-6:00pm
Wednesday 8:00am-6:00pm
Thursday 8:00am-6:30pm
Friday 8:00am-7:20pm
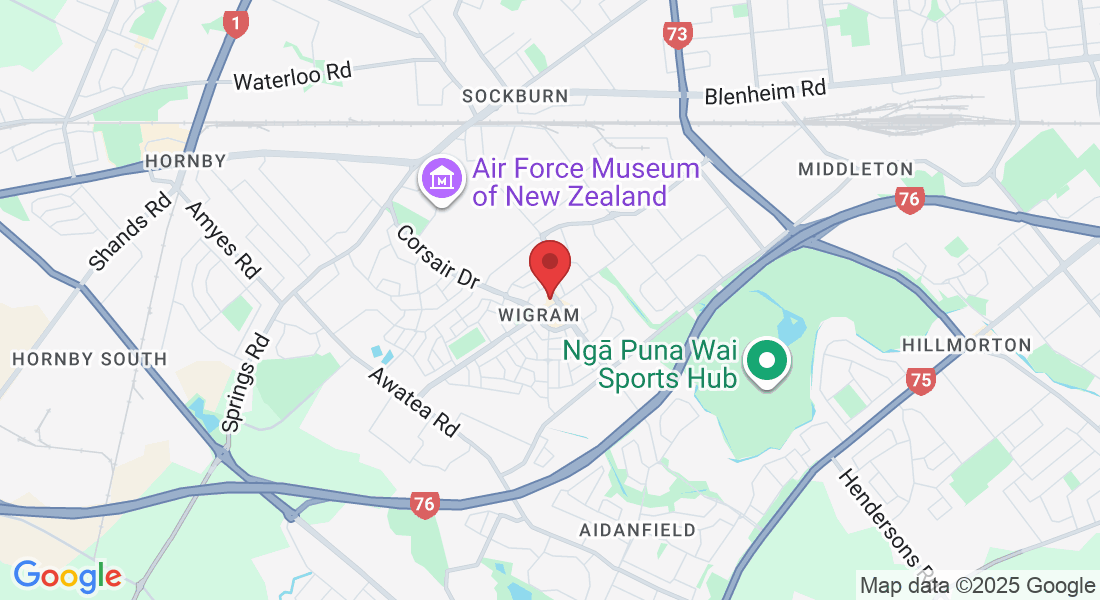
Wigram
03 322 9400
67 Skyhawk Rd, Wigram, Christchurch 8042
Monday 8:00am-8:00pm
Tuesday 9:00am-6:00pm
Wednesday 8:00am-8:00pm
Thursday 8:00am-8:00pm
Friday 8:00am-7:20pm


© Copyright 2026 Vitala Health. All Rights Reserved.
Facebook
Instagram
LinkedIn